Technology in health care – startup challenges & industry insights

Nowadays, technological development in medicine is one of the most interesting fields of software development. It’s becoming more and more obvious that modern medical technology is not only about medical equipment, machines, and devices. The move forward is strongly noticeable in the context of modern medical software and the possibilities offered by access to medical information and data online.
In this article, you’ll learn how implementing digital technology in the healthcare industry can improve the healthcare experience for medical staff, patients, and organizations. You’ll also find out what challenges you may encounter when developing a startup product.
This post contains my observations from the time I spent creating digital health startup products as a JS developer. These insights will be food for thought that will help you develop better healthcare technology solutions.
What is healthcare technology?
According to IBM’s definition, it is any technology, including medical devices, IT systems, algorithms, artificial intelligence (AI), cloud, and blockchain, designed to support healthcare organizations.
Benefits of healthcare technology
We can split benefits by the groups of people contributing to or participating in the healthcare system.
Healthcare providers
The first group is healthcare providers: physicians of any specialty, nurses, or clinical social workers. Potential benefits include:
- Easier access to health records. Healthcare professionals could easily access medical records from previous appointments, other organizations, or specialists.
- Faster and more accurate diagnosis process. Providers could see any lab results, historical assumptions, or past vital levels. A smart application could also advise which record is key-finding and should be investigated deeper.
- Less time spent working on documentation. The repetitive part of work, which is not providing health care directly, could be automated.
Patients
The second group is patients. Potential benefits include:
- Easier access to healthcare providers. Patients could chat with their physicians, solve problems that can not wait until they visit the doctor, or clarify appointment conclusions. All health data could be immediately transferred between institutions when patients decide to change their providers.
- Patient records analysis. Patients, in cooperation with medical professionals, would be able to analyze which initiatives could improve their state of health. For example, a mobile app could send them notifications and reminders about the health goals they’ve set. Such a solution would make it easier for patients to stick to these goals.
Pharmaceutical industry
The third group is pharmaceutical companies. Potential benefits include:
- Product improvement. Many research centers or pharmacy companies currently use anonymized patient data obtained from healthcare technology solutions to improve their products.
Research centers
The fourth and final group includes research centers. How can they benefit from healthcare technology development?
- Opportunity to analyze population health records. Access to such vast data might result in various interesting conclusions, for instance, ground-breaking discoveries regarding illness triggers or population determinants.
💡 [DIGITAL HEALTH CASE STUDY]
WithHealth: Releasing a fully operational patient MedTech portal in just 6 weeks in response to the COVID-19 pandemic
Technology in the healthcare industry
There are many technologies used in the healthcare industry. However, I’ve decided to focus on those I know best.
Machine learning
With well-structured and qualitative data, you can build interesting machine-learning models. Quantitative data has become increasingly important because of the high demand for the predictions that it can produce. Machine learning is a game-changer in the field of health technology, but it poses some challenges.
CHALLENGES:
- First of all, you must possess as much data about the patient as possible. Otherwise, the data model use case will be limited.
- If your product implies using data from different sources, you’ll need to convert it to the same data structure. The conversion can be very tricky or sometimes even impossible.
- If there’s data that hasn’t yet been digitized, you will have to manually enter it into your database, which might be expensive and time-consuming.
- You can’t rule out the fact that the data might be unreliable. The reason for this might be mistakes made by healthcare workers while entering the data or deliberate falsification of data by the patient.
- Poor process of data validation.
- Data classification based on different standards, e.g., SNOMED CT Problem List vs. ICD-10-CM/PCS HIPAA Code Sets.
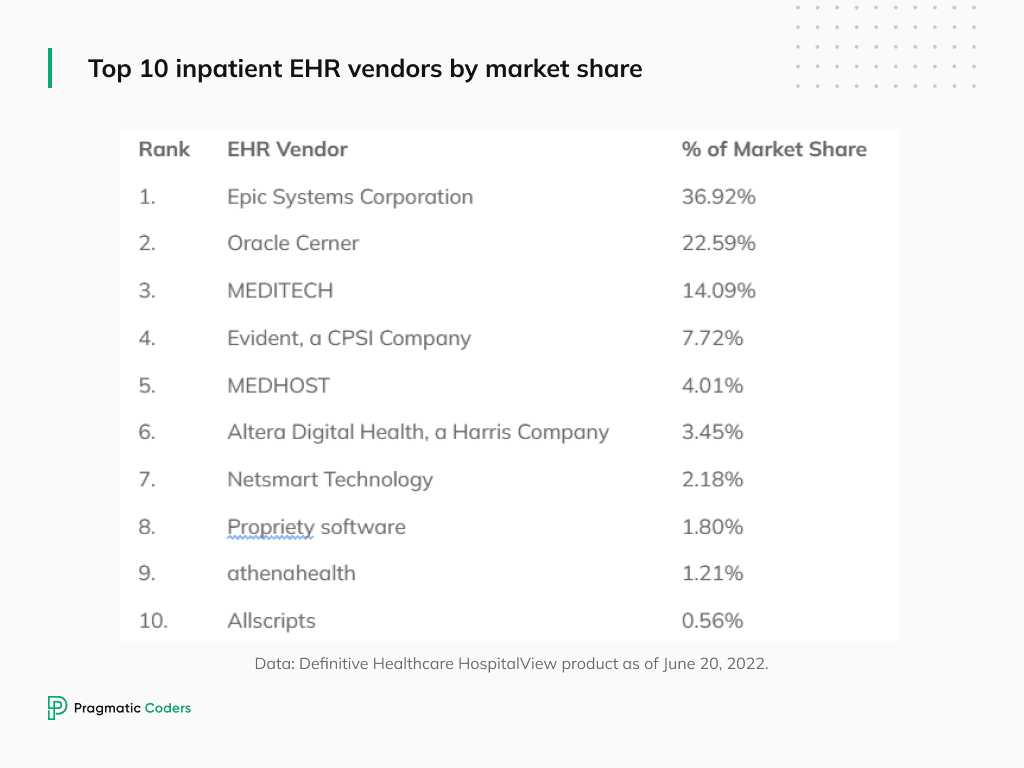
Electronic health records
Electronic health records (EHRs) are digital versions of traditional paper-based medical records. They allow medical providers to manage patient information in an organized and secure way, enabling them to better care for their patients and improve the overall quality of care. EHRs contain a wide range of data about each patient.
- Allergies (name, reactions, severity, onset date, last occurrence)
- Activities, e.g., meditation or physical activities (name, duration, frequency, effort level)
- Diets, e.g., meals or dietary plan (name, frequency, calories level)
- Lab results (type, unit, result, abnormality level, procedure date)
- Genetic data (gene name, abnormality level, procedure date, result, inheritance, trait, illness related)
- Vitals (kind, value, unit, occurrence date, abnormality level)
- Social History (type, value, observation date)
- Mental Health (question, value, observation date)
- Microbiomes for culture, labs, parasitology, zone, stool (name, score, unit, interpretation, abnormality level, test date)
- Illnesses (name, onset date, deactivated date)
- Sleep information (type, value, observation date)
- Meds and Supplements (name, dosage, prescribing physician, sig, unit, start date, end date, reason)
- Drugs (type, value, start date, end date)
- Surgeries and hospitalization history (name, procedure date, reason, location)
- Goals and challenges (name, comment, start date, end date)
EHRs are a critical piece of technology for most healthcare facilities as they serve as a digital record system for patient healthcare data.
CHALLENGE: Healthcare provider organizations, like hospitals, generally have various computer systems used for a variety of purposes, from managing billing records to patient tracking. Ideally, these systems should interface with one another when inputting or extracting information, enabling a data-driven approach to healthcare. However, this is not always the case.
SOLUTION: Applying data standards.
The most broadly used data standards in the healthcare industry are Health Level 7 (HL7) standards. In the last years, there were 3 most popular data representation standards:
Health Level 7 (HL7) Version 2
HL7 Version 2 is the most widely used healthcare messaging standard for exchanging clinical and patient information between systems. With no other standards available at the time, a custom HL7v2 format was created based on pipe and hat encoding and has continued to be developed “ad hoc” over the years.
All v2.X versions maintain backward compatibility to ensure the legacy and modern applications can communicate simply by ignoring unexpected content or repetitions. The HL7v2 standard is not a complete plug-and-play solution for interoperability, and it is often referred to as the “non-standard standard” as it provides around 80% of the interface foundation, with 20% still requiring some customization on an interface-by-interface basis.
Each hospital, urgent care center, ambulatory care facility, imaging center, laboratory, and other care facility have unique clinical systems and operations, making each implementation of HL7 requires a slightly unique representation of the data.
Health Level 7 (HL7) HL Version 3
HL7 Version 3 (including the most popular HL7 CDA) was developed over a 10+ year period using lessons learned and best practices from previous versions with the goal of creating a more firm and context-rich standard that supports healthcare workflows through the exchange of data between healthcare organizations and providers.
HL7 developed v3 based on a methodology of shared models, the Reference Information Model (RIM), enabling more reuse, standardization, and format consistency. XML is used as the message syntax for a more human-readable but larger message. Due to several reasons, including its complexity and the fact that HL7v3 is not backward compatible with HL7v2.X.
Fast Healthcare Interoperability Resources (FHIR)
Fast Healthcare Interoperability Resources (FHIR) defines how healthcare information can be exchanged between different computer systems regardless of how it is stored in those systems. It allows healthcare information, including clinical and administrative data, to be available securely to those who have a need to access it and to those who have the right to do so for the benefit of a patient receiving care.
FHIR’s development began in 2012 in response to market needs for faster, easier, and better methods to exchange the rapidly growing amount of health data. This growth in the availability of new health data, along with the progressing “app” economy, created the need for clinicians and consumers to be able to share data in a lightweight, real-time fashion using modern internet technologies and standards.
FHIR is based on internet standards widely used by industries outside of healthcare. In particular, these include the REST approach, which describes how individual packets of information (termed Resources) can be shared easily. By adopting existing standards and technologies already familiar to software developers, FHIR significantly lowers the barriers of entry for new software developers to support healthcare needs.
💡 [DIGITAL HEALTH CASE STUDY]
AccentPharm: Building an innovative Linguistic Quality Assurance app in just 8 weeks
Administrative health tech
Administrative health tech is a term used to describe the use of technology to increase hospital and administrative productivity and reduce growing administrative workloads. It includes the implementation of various software applications and systems that automate, streamline, and simplify administrative processes in healthcare facilities.
With all I said before about automatization and data standards, there will still be cases when digital solutions aren’t enough. Human errors, automation mechanics failures, lack of digitalized data, or missing data contribute to the need for manual support.
CHALLENGES:
- Every patient survey answer should be verified by some sort of care coordinator.
- Data can come from systems that use old data representation standards. Administrative personnel needs to determine how to classify each patient record. For example, some systems return med information combining sig(1), dosage, unit, and name information, while others split it.
- Image or pdf recognizers might fail or return inaccurate information, so it needs to be verified on a sample at least.
- Automation mechanics inside an application that determine the abnormality level or key-finding observations might fail in corner cases.
- Even the newest FHIR standard does not provide all the information, e.g. some code could be missing.
- Physicians may make mistakes (even simple spelling mistakes) when writing patient notes or any other type of medical documentation. Such documents should be then reviewed to ensure the data is valid.
- Patients could come with paper documents describing historical information; in that case, someone needs to manually input it into the application.
- It would be great if developers had a perfect understanding of how the medical industry works and what its demands are (from what patients need to the latest legal requirements). The reality is they don’t. Then, it’s a good idea to have someone monitor the changes in the industry and update the product development team.
SOLUTION: Manual support
(1) The abbreviation “Sig” stands for “let it be labeled.” This important instruction can often be found in prescriptions preceding the directions. It informs the pharmacy of what to include on the drug’s label, ensuring you understand how and when to safely take your medication. Examples: “TID” = “three times a day”, “QD” = “once a day.”
Conclusions
Digital technology has revolutionized the way we live our lives. It has transformed the way we work, play, and communicate. And now, it is beginning to change the way we receive healthcare.
I hope this post gave you a hint about healthcare technology and the challenges you may encounter when dealing with machine learning, patient records data or administrative healthcare.
Have any questions? Feel free to contact us!