Pros and Cons of Telemedicine and Telehealth Services
Today, healthcare services are at their most accessible. No matter where you are, a doctor’s appointment is just a few clicks away. Telemedicine and telehealth, blending technology with healthcare, make this possible. This journey started way back. Think 1800s, when home-based care was a budding idea. By 1879, an article in The Lancet talked about treating patients over the phone. Fast forward to 1925, and doctors were diagnosing illnesses via radio. The leap to video calls? That happened in 1959 at the University of Nebraska.
This article dives into the pros and cons of telehealth, exploring the ups and downs of this game-changing approach to healthcare. We’re here to highlight how telemedicine systems are reshaping the way we think about medical care. Plus, we’ll sprinkle in some intriguing stats to paint a clearer picture.
The concept of telemedicine
To start things off, let’s get into what telemedicine actually is. At its core, it’s about delivering medical advice, diagnoses, and treatment through digital platforms. It’s healthcare powered by your smartphone or computer.
It started simple. Back in the day, it might’ve been a call to a nurse about a fever. Now? It’s video chats with specialists, text updates to your doctor, and apps that keep an eye on your health. It’s healthcare catching up with the digital age, bringing you virtual care. Telemedicine is at the forefront of digital health trends, shaping the future of how we receive healthcare.
What’s great about it is how it fits into your life. Got a quick question? Fire off a message. Managing something more serious? Regular video check-ins can keep you on track without the hassle of visits. It’s all about making healthcare work for you, not the other way around.
Facts and figures about telemedicine
The COVID-19 pandemic threw telehealth into the spotlight. As clinics closed and the world went online, these services weren’t just convenient; they were essential. Here at Pragmatic Coders, we played a role in this pivotal transition. The following facts highlight telemedicine’s success, but they also point to some problems.
Telehealth usage and trends
Pre-pandemic, telehealth was on a steady climb. Then COVID-19 hit the fast-forward button, increasing remote health visits by 38 times from the baseline. Rural areas saw 147 visits per 1,000 patients, while urban spots had 220. Post-pandemic, the numbers dipped but remained significantly higher than before, with 22% of U.S. adults using telehealth from April to August 2021.
Consumer preferences and demographics
About 80% of people have tried telemedicine once, showing its wide acceptance. Interestingly, 76% of those over 55 have used telehealth services, challenging the notion that older generations shy away from tech. Millennials and rural residents are also on board, with high percentages favoring virtual visits.
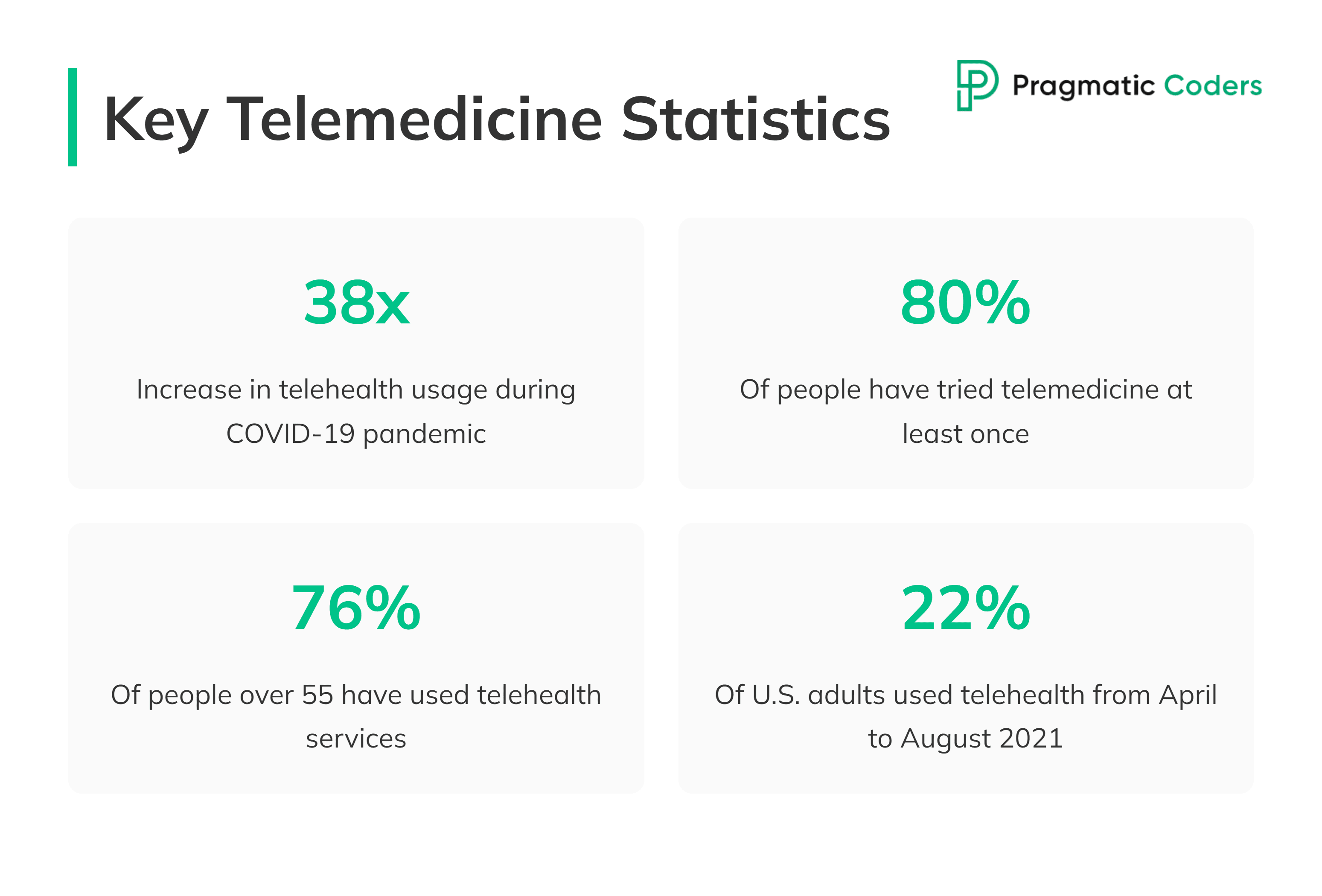
Telehealth challenges and satisfaction
While telehealth has its proponents, hesitancy remains. Concerns over cost, risk, and satisfaction highlight areas needing improvement. Yet, many healthcare providers found telemedicine invaluable, with a significant portion of patient visits remaining virtual post-pandemic. This balance of challenges and successes paints a complex picture of telemedicine’s role in our lives.
Pros of telemedicine
Sure, telemedicine got a boost from recent world events. But let’s think about it: how much was due to sheer circumstance, and how much is because it’s truly groundbreaking? Let’s take a closer look at the benefits of using telemedicine services.
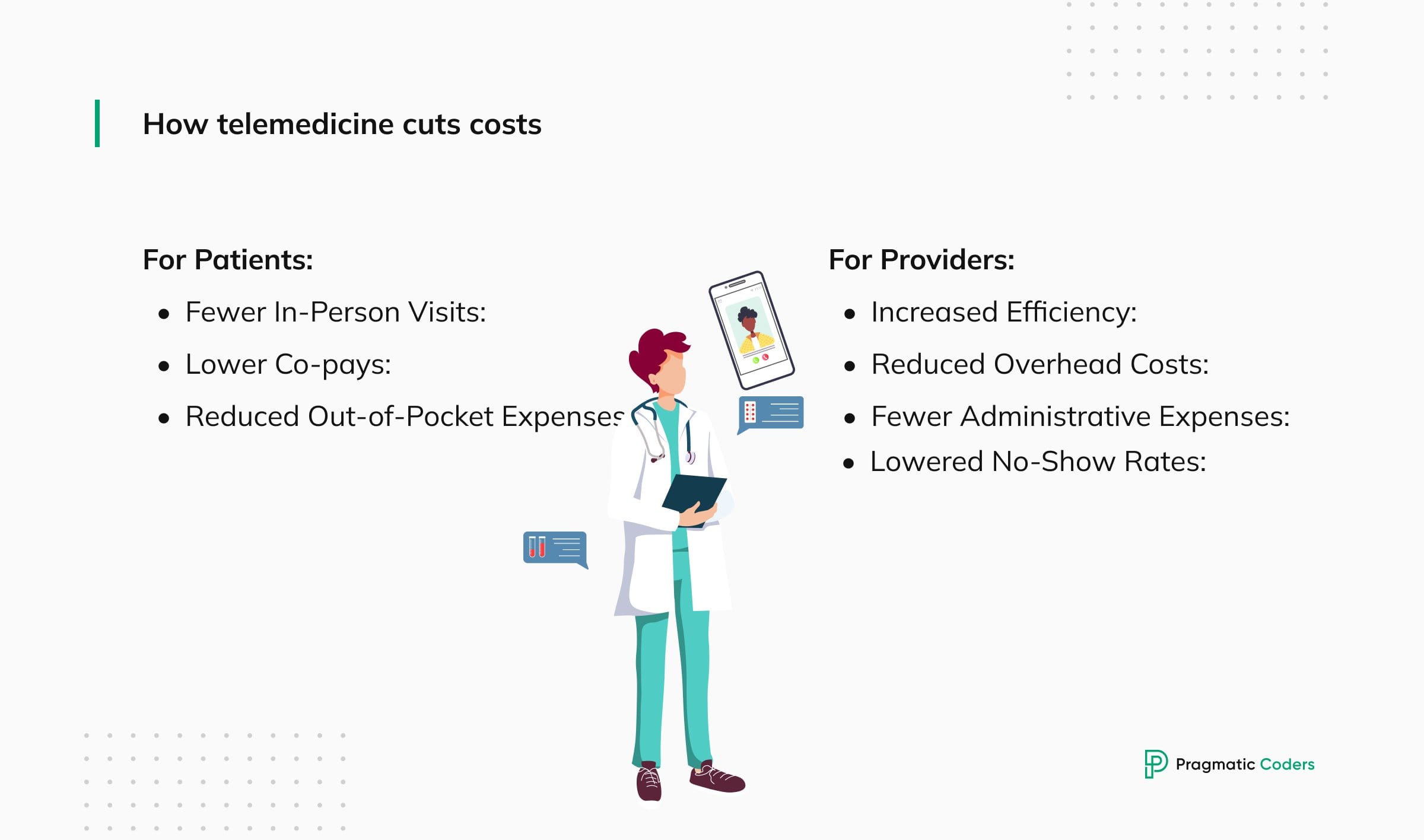
Cost savings
Telemedicine is a game-changer for everyone’s wallet. It’s about more than saving on gas money. Virtual consultations and remote monitoring cut down on unnecessary ER visits, reducing healthcare costs for both patients and providers. For instance, a simple video call can replace a costly in-person visit for routine follow-ups.
Here’s a quick breakdown of how telemedicine cuts costs:
For Patients:
- Fewer In-Person Visits: Say goodbye to travel, parking fees, and taking time off work for routine check-ups or medication refills. Virtual consultations have got you covered efficiently.
- Lower Co-pays: Many insurance plans are now offering lower co-pays for telemedicine visits, making them even more wallet-friendly compared to in-person consultations.
- Reduced Out-of-Pocket Expenses: Skip the emergency room visits for minor issues that a virtual consultation can easily handle. Plus, early intervention via remote monitoring can keep more serious (and expensive) complications at bay.
For Providers:
- Increased Efficiency: Doctors can see more patients remotely, making the most of their time and streamlining clinic operations.
- Reduced Overhead Costs: With telemedicine, the need for extra office space goes down, along with rent, utilities, and upkeep expenses.
- Fewer Administrative Expenses: Things like scheduling appointments and follow-up chats become simpler, lightening the load on staff and cutting costs.
- Lowered No-Show Rates: Telemedicine appointments tend to have fewer no-shows. It’s easier for patients to fit them into their day, reducing wasted time and resources.
Interested in harnessing these benefits for your healthcare practice? Discover our telemedicine software development services. Let’s innovate together to make healthcare more accessible, efficient, and cost-effective.
Convenience, accessibility, and reach
Telemedicine makes clinical services more accessible and convenient than ever before. It eliminates the common barriers of distance, time, and mobility, bringing top-notch primary care right to your doorstep. By closing this gap, telemedicine simplifies the process of connecting with digital doctors, regardless of your location. It serves as an essential link for areas that lack local healthcare services.
Here’s how telehealth solutions are increasing convenience, accessibility, and reach of care:
Convenience at Your Fingertips
- Schedule Flexibility: Forget about waiting rooms or rescheduling because of work or personal commitments. Telehealth offers appointment times that suit your busy life.
- Location Independence: Get consultations from anywhere – home, office, or on the move. It’s a game-changer for those in remote areas or with mobility challenges.
- Reduced Travel and Waiting Time: Cut out travel costs and time, along with all the waiting room hassle.
- Improved Caregiver Support: Caregivers can join in on consultations remotely, leading to better communication and teamwork in care planning.
Accessibility for All
- Bridging the Distance Gap: Now, people in rural places or those with limited transport options can access leading healthcare specialists from anywhere.
- Empowering Individuals with Disabilities: Those with physical challenges or chronic conditions gain more independence in managing their health, lessening the need for help with transport.
- Breaking Language Barriers: Connect with healthcare providers who speak your language for clear communication and better decision-making.
- Improved Mental Health Access: Telemedicine offers a more discreet and less daunting way to access mental health services, encouraging early help-seeking.
Increased Reach for Underserved Communities
- Specialist Consultations: Now, patients in remote or specialist-limited areas can reach out to experts far away. Telemedicine closes that gap, bringing specialist care to those who previously had little access.
- Shortage Relief: It’s also addressing healthcare provider shortages, especially in rural spots. Remote consultations support local doctors, ensuring even the least served communities get quality care.
- Improved Continuity of Care: Those living far from healthcare facilities can now have steady care without the travel trouble, thanks to telemedicine.
- Eliminating Transportation Challenges: For anyone facing travel woes or mobility issues, telemedicine means healthcare can be accessed without leaving home.
Personalized care and remote monitoring
Telemedicine isn’t one-size-fits-all. It adapts. Whether it’s a real-time video chat, a message about your symptoms, or devices that monitor your health from afar, telehealth tailors to your needs through data-driven healthcare. Take, for example, a patient with chronic heart disease. Remote monitoring (or, if we go one step further, ambient health monitoring) allows their doctor to keep tabs on their health daily, adjusting treatment without the need for an in-person visit. These innovations are not just changing how we access healthcare; they’re improving the quality of life.
Cons of telemedicine
Although telemedicine revolutionizes healthcare, it’s not without its flaws. Let’s explore the other side of the coin by delving into the challenges and disadvantages of telemedicine.
Lack of physical examination
One major hiccup? The absence of in-person exams. It’s tough to replace the hands-on assessment a doctor can provide face-to-face. This gap can lead to worries about missed diagnoses or not fully understanding a patient’s condition. Plus, there’s something about physically seeing a doctor that feels more personal. We’re social creatures, after all.
Privacy and security risks associated with telemedicine
Then there’s the digital dilemma. With more data online, the risk of privacy breaches climbs. Despite strong security measures, the thought of sensitive health information floating in the digital ether is unsettling. It’s a reminder of the constant battle between innovation and privacy.
Here’s a detailed look at the potential privacy and security risks associated with telemedicine:
- Data Breaches: The digital world is full of cyber threats. When patient info is sent online or stored on EHRs (Electronic Health Records) systems, it’s at risk. A hacker getting their hands on your medical records could lead to serious problems, like identity theft or even discrimination based on your health. Adding another layer of defense in the form of data tokenization can help protect your sensitive data in case of a data breach.
- Slip-Ups: We’re only human, and mistakes happen. A typo here or a misstep in sending data can accidentally give the wrong people access to sensitive info.
- Third-Party Hiccups: Telehealth doesn’t just involve you and your doctor; there are also tech companies and data storers in the mix. If any of these players have a security slip, your data could be at risk.
- Security Shortfalls: For telemedicine to be safe, everyone involved needs top-notch security measures. If the systems aren’t up to scratch—with weak passwords, old software, or a team that’s not clued up on cyber safety—patient data could be left hanging in the breeze.
Technological barriers between patients and remote healthcare providers
Tech can be tricky, especially for those not born with a smartphone in hand. Older patients may find navigating telemedicine platforms challenging, widening the digital divide. But it’s not just an age thing; access to reliable internet and devices also plays a big part.
Here are some of the hurdles we’re facing:
Digital Literacy and User Interface Challenges:
- Navigating Platforms: For folks not too savvy with tech, telemedicine platforms can seem like a maze. Clunky interfaces and tech jargon can throw up roadblocks to care. What we need are user-friendly designs that guide users smoothly, with clear directions and helpful tutorials to ease the way.
- Limited Digital Literacy: It’s not just about the young and techy. Older adults or those not up to speed with the latest gadgets might find even basic tasks tricky. Think downloading apps or hopping onto a video call. Telehealth needs to step up, offering solid training and support, maybe even a chat on the phone, to get everyone on board.
Access to Technology and Infrastructure:
- The Affordability Gap: Not everyone’s pocket stretches to smartphones, tablets, or computers – the essentials for telehealth. How about subsidized gadgets or teaming up with community hubs to make sure everyone’s in the loop?
- The Connectivity Divide: Smooth telemedicine sessions need steady internet, but that’s not a given everywhere. The gap in net access and speed is wide, especially off the beaten track. It’s high time for an investment boost in broadband, aiming to get every corner connected.
Regulatory and legal complexities of telehealth systems
The legal landscape of telemedicine is like a maze. With different rules across states and countries, it’s a headache for providers to stay compliant. Licensure, reimbursement, and liability add layers of complexity. Yet, as tricky as it is, navigating this maze is crucial for telemedicine’s growth.
Here are some examples illustrating these complexities:
- Licensure Challenges: Crossing State (and International) Borders
- Example: Dr. Jones, a licensed physician in California, wants to provide telemedicine services to patients in Nevada. However, Nevada has different licensing requirements. Dr. Jones must navigate the state-specific rules to ensure compliance. Also, this gets much more complicated when international borders come into play…
- Reimbursement Policies: Payers and Coverage
- Example: Telemedicine reimbursement varies across payers (private insurers, Medicare, Medicaid). Dr. Smith, a psychiatrist, offers virtual counseling sessions. Medicare covers some services, but private insurers differ. Dr. Smith needs to verify reimbursement policies for each patient.
- Liability Concerns: Standard of Care and Malpractice
- Example: Nurse Practitioner Rodriguez provides telemedicine consultations. A patient alleges negligence, claiming inadequate advice during a virtual visit. The question arises: What is the telehealth standard of care?
- Privacy and Security Compliance: HIPAA and Data Protection
- Example: Dr. Curtiss conducts video consultations. During a session, the patient’s sensitive health information is accidentally visible to family members. Dr. Curtiss faces potential HIPAA violations. How to avoid this? Check our guide to HIPAA-compliant software development for a detailed answer.
- Telehealth Interstate Compact (TIC): Streamlining Licensure
- Example: The TIC allows licensed providers to practice across participating states. Dr. Garcia, a psychiatrist, joins the compact. Now she can offer telepsychiatry services to patients in multiple states without individual licenses.
Telemedicine’s true influence on healthcare
We’ve covered the pros of telemedicine. We’ve tackled the cons. Now let’s see the end result.
Virtual visits cut travel time. Yet they reduce face-to-face contact. Remote health monitoring systems track vital signs. They support better coordinating care at a distance. Online portals and patient portals give quick access to exam notes and test results. They make appointments simpler. Some clinics use chatbots for triage. These bots handle basic questions and direct patients to the right service.
Doctors also rely on store-and-forward video conferencing to share images or documents. This form of provider-to-provider communication can save time, but it lacks real-time feedback. Consumer adoption of telemedicine continues to grow. Many patients embrace virtual care and video calls for routine check-ups. Yet some miss the human warmth of in-person interactions.
Telemedicine’s true impact lies in how well we balance new tools with personal contact. While it can boost access, trust and familiarity matter, too. By refining the digital experience, we can build a future where telehealth meets patients’ needs while preserving the human side of healthcare.
Future trends in telemedicine services
Despite its challenges, telemedicine is set to play a starring role in the evolution of healthcare. Its integration into existing systems promises to make healthcare more seamless and efficient.
Integration with healthcare systems
The future of telemedicine looks incredibly promising. It’s evolving from a nice-to-have feature into a central element of healthcare systems. Picture a world where immediate access to a doctor through a virtual visit is the norm. Plus, imagine that doctor having seamless access to all your health records. Accessibility, integration, and the highest quality of care; that’s where telemedicine is heading.
Research and innovation in telehealth services
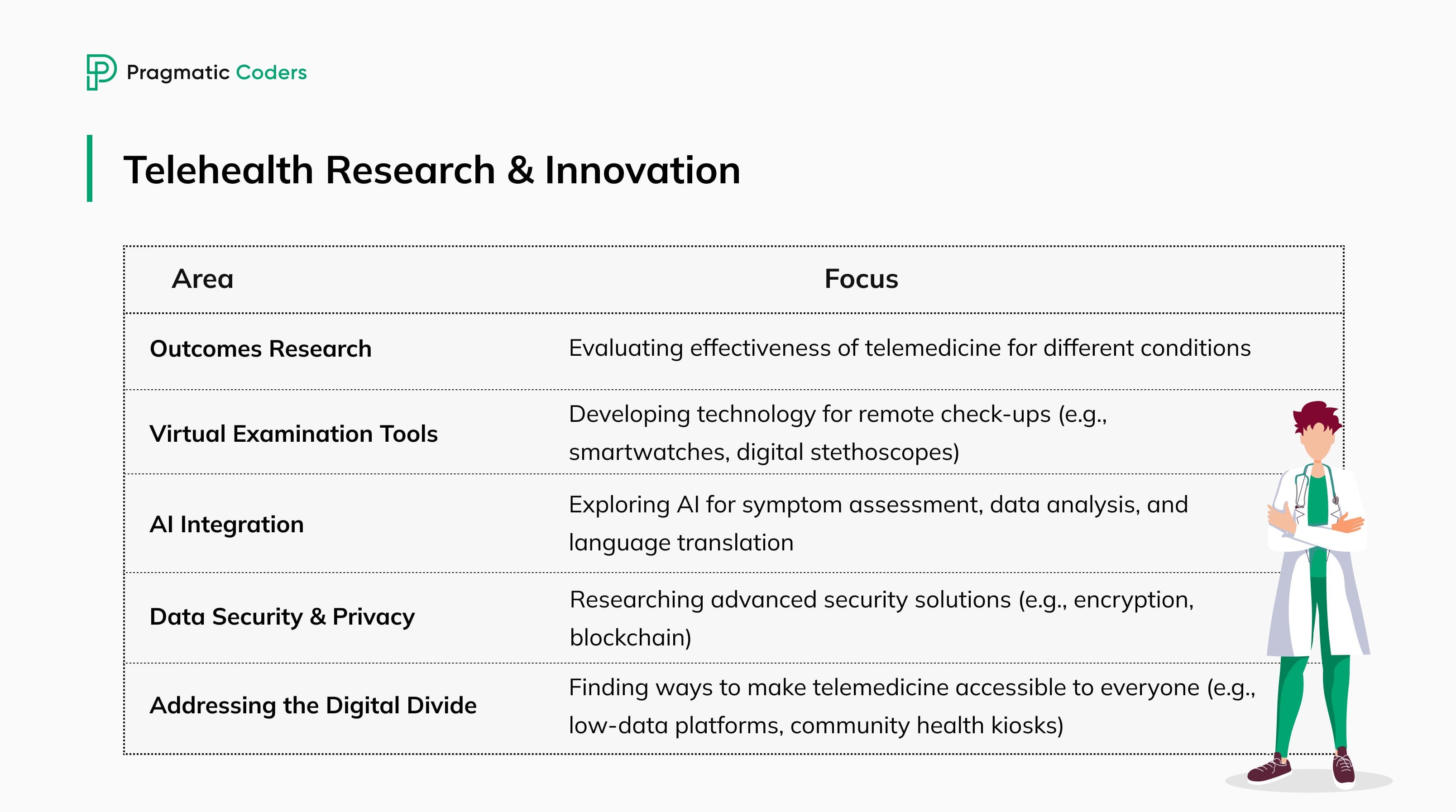
Promoting research in telehealth is crucial for its advancement. There’s still so much to learn. Below are some key areas for exploration:
- Outcomes Research: We need to dig deep and see just how effective telemedicine is for various conditions. Can virtual chats really stand up to face-to-face sessions for tackling anxiety? What about remote monitoring for heart disease – does it make a long-term difference? Through solid research, we’ll find the answers, shaping the best ways to care for patients digitally.
- Virtual Examination Tools: Sure, telemedicine can’t offer a hands-on check-up yet. But, the wheels of innovation are turning. Imagine strapping on a smartwatch that does more than count steps, or a digital stethoscope that lets your doctor listen in from miles away. Advances in tech could soon make thorough virtual check-ups a reality.
- AI Integration: AI is set to revolutionize telemedicine. Picture a smart chatbot that sorts out your symptoms before you even see a doctor. Or AI that makes sure nothing gets missed in your health data. It could even break down language barriers in real-time. As we explore AI further, we’re opening doors to smarter, more personalized, and accessible care.
- Data Security and Privacy: With more of us clicking to see our doctor, keeping our data safe is more important than ever. Investigating cutting-edge security, like unbreakable encryption or blockchain, will help keep our health info secure and private. This is key to keeping trust in telemedicine strong.
- Addressing the Digital Divide: Not everyone’s online life is created equal. We need smart solutions to make sure everyone can hop on the telemedicine train. Research into low-data platforms or community health kiosks could ensure that tech doesn’t leave anyone behind. Let’s make sure telemedicine benefits all, not just the tech-savvy.
Conclusion
At first glance, telemedicine might seem like a bit of a mixed bag. On one hand, it offers cost savings, convenience, and extended reach. On the other, it grapples with challenges like the lack of physical exams, privacy concerns, and the digital divide.
But here’s the thing: the pros far outweigh the cons. With careful attention and ongoing improvement, telemedicine can continue to transform healthcare. It’s about striking the right balance, enhancing what works, and fixing what doesn’t.