Future of healthcare: 2026-2040

There are 3 main statements we can make based on the healthcare trends we observe:
- Mental health — it’s getting worse.
- Aging — there are more and more older people, who are also getting older and older.
- Human+ — technology is increasingly used to eliminate or reduce diseases and disabilities.
So what do we do about it? As a humanity, we somehow need to cope with these shifts. Below I present 14 health-related trends that will shape the way we function over the next 15 years.
Source: The entire article is rooted in infuture institute’s Trend Map – a comprehensive picture of social, technological, environmental, economic and political change.
Cluster: Mental health & social fabric
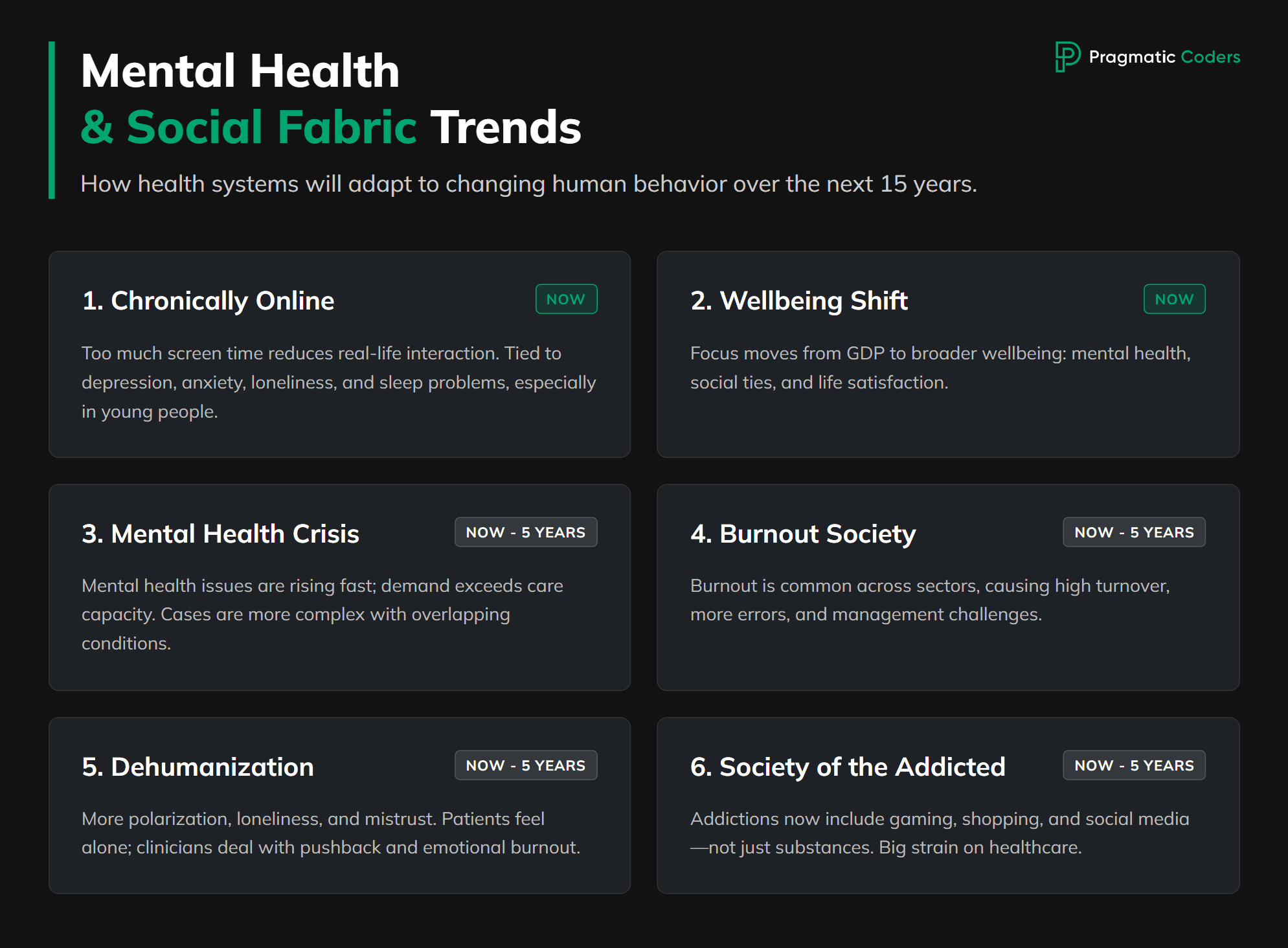
Over the next 15 years, health systems won’t just be treating “more depression and anxiety”. They’ll be dealing with an entire shift in how people live, relate and cope.
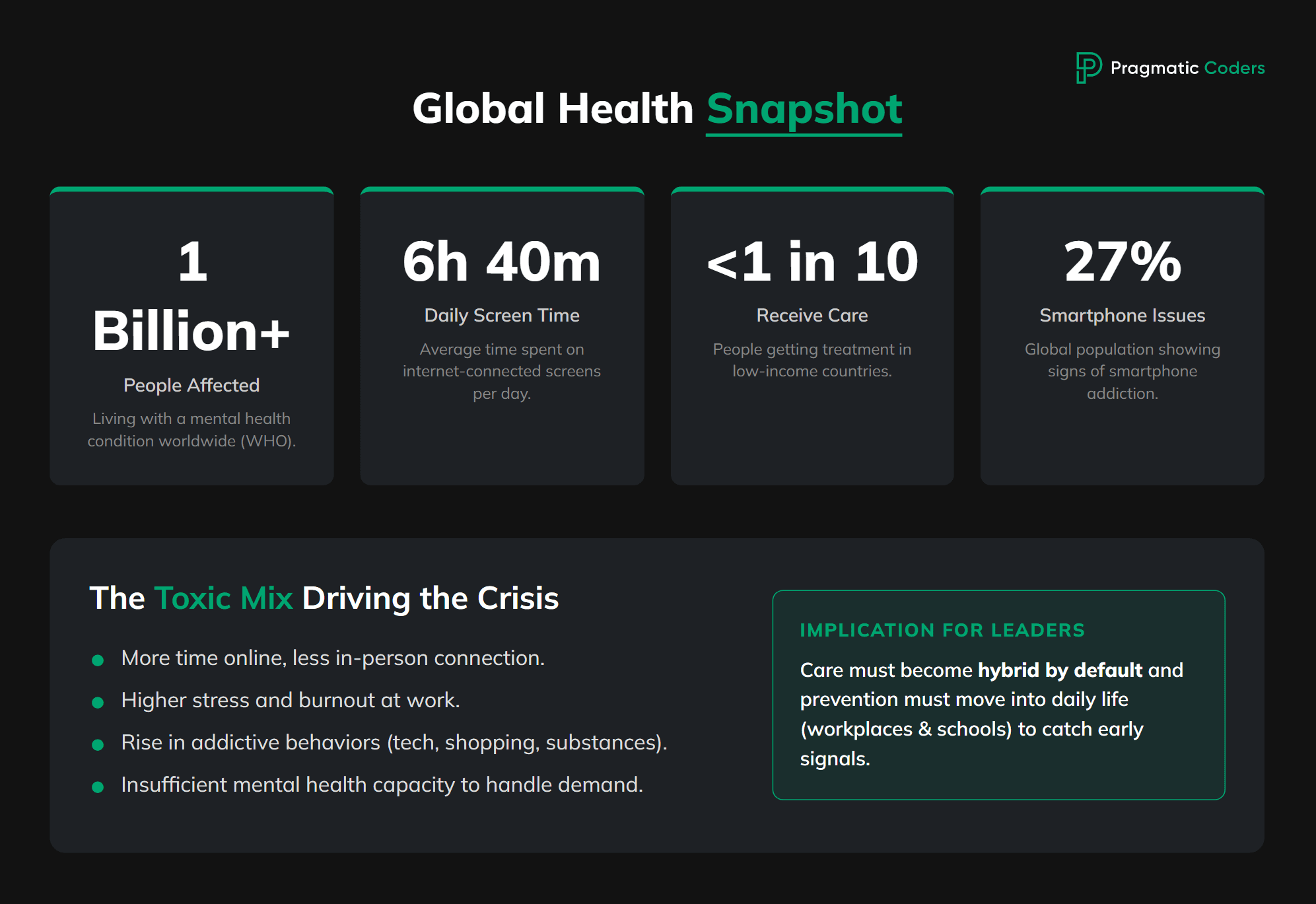
A few numbers to anchor this:
Over 1 billion people are now living with a mental health condition worldwide, according to the latest WHO data. Mental disorders are already one of the leading causes of disability globally.
Most of them don’t get proper care – in low-income countries, fewer than 1 in 10 people with a mental health condition receive treatment. (Health Policy Watch, 2025)
At the same time, people now spend about 6 hours and 40 minutes a day on internet-connected screens (phone, laptop, tablet, TV). That’s a big chunk of our waking life happening online. (Exploding Topics, 2025)
A large meta-analysis found that around 14% of the global population shows signs of internet addiction, about 27% for smartphone addiction, and around 6% for gaming addiction. (ScienceDirect, 2021)
So you get a powerful mix:
more time online,
weaker in-person social networks,
higher stress and burnout at work,
more addictive behaviours (substances, tech, shopping, gambling),
and not enough mental health capacity to handle all this.
For healthcare leaders, this cluster (Chronically Online, Wellbeing, Mental Health Crisis, Burnout Society, Dehumanization of Relationships, Society of the Addicted) means three big things:
Demand will keep rising and changing shape
More patients arrive with complex, overlapping problems: depression + anxiety + addiction + sleep issues + loneliness.
Causes are often tied to work pressure, digital life, financial worry and social isolation, not just “classic” psychiatric diagnoses.
Care has to be hybrid by default
Patients expect digital entry points (apps, chat, video) and meaningful human contact.
Many will only accept help if they can start online and stay mostly online, especially younger people.
Prevention and early signals move into daily life
Early warning signs show up in workplaces, schools, and digital behaviour long before someone shows up at a clinic.
Health systems that connect clinical care with employers, schools and digital tools will catch problems earlier.
The trends in this cluster are basically different “faces” of the same reality:
a world that is more connected, more pressured, more online – and more mentally fragile.
| Patient portal development services Custom patient portal solutions designed for efficiency, accessibility, and enhanced patient engagement. Learn more. |
Trend 1 – Chronically Online (NOW)
What’s specific here?
People, especially teenagers and young adults, spend so much time online that it starts to replace real-life contact. They socialise, argue, date, learn and work through a screen. Heavy social media and gaming use is linked with higher rates of depression, anxiety, loneliness and sleep problems, and for a part of the population it crosses into addictive patterns of use.
Signals you’ll see in your organisation
Different symptom patterns in younger patients
Mood swings tied to online events: break-ups, bullying, group chats, “cancelling”, gaming conflicts.
Strong link between night-time screen use and insomnia, fatigue and low mood.
Patients who are “socially active” but deeply lonely
Many followers, many chats – but no close offline relationships, very little local support network.
Trouble with basic in-person skills: eye contact, small talk, conflict resolution.
Digital channels under pressure
Your chat, helpline or portal gets used for emotional crisis and mental health venting, not just admin questions.
Staff feel unsure how far they should go in messaging before it becomes “therapy in the inbox”.
What to consider in the next 12–24 months
Ask about digital life as a standard part of intake
Add a few simple questions:
“How many hours a day do you usually spend online outside work/school?”
“Do you often stay up late because you’re on your phone or computer?”
“Do conflicts or things that happen online affect your mood a lot?”
Treat these answers as risk flags, just like smoking or alcohol use.
Design safe digital-first paths for mental health
Make it easy to start with self-assessment + chat or short video visit.
Define clear rules for:
when to move someone from chat to a full consult,
when to invite them onsite,
what counts as an emergency and how to escalate.
Adjust your digital products to real mental-health use cases
If you have (or plan to build) your own patient app / portal / platform, make sure it can:handle asynchronous messaging with clear response times,
show simple, evidence-based content on sleep, anxiety, comparison and social media stress,
connect easily with your scheduling, records and telehealth tools.
Support your staff, not just patients
Train clinicians and support teams on how to:
talk about screen time without blaming,
respond to crisis-like messages in chat,
set healthy digital boundaries (no constant 24/7 messaging expectation).
Discover how Health Folder revolutionizes medical documentation management with its AI-powered mobile app built using low code.
Health Folder: Your AI-based digital medical documentation folder
Trend 2 – Wellbeing (NOW)
What’s specific here?
“Wellbeing” is the counter-movement to all the stress, pressure and digital overload. Governments and organisations are slowly shifting from “GDP only” to broader wellbeing metrics – including mental health, social connection and life satisfaction. The OECD, UN and others now use multi-dimensional wellbeing frameworks to track how people are actually doing, not just how much they produce. (OECD)
Signals you’ll see in your organisation
Employers and payers start asking for wellbeing outcomes, not just claims data
HR and insurers talk about burnout, life satisfaction, stress, loneliness.
More interest in preventive programs and lifestyle support (sleep, activity, diet, stress).
Patients expect “whole person care”
Not “here’s your prescription, goodbye”, but support that touches work, family, sleep, habits, digital life.
More demand for coaching, group programs, lifestyle medicine and mental health support around chronic disease.
What to consider in the next 12–24 months
Add simple wellbeing indicators to your patient and population data
Short questions about life satisfaction, stress, loneliness, sleep quality.
Use them to segment patients and design more tailored programs (e.g. “high medical risk + low wellbeing”).
Build or partner for wellbeing programs around your core medical services
Example: diabetes or cardiac rehab programs that include sleep, stress, movement and mental health modules, not only medication and diet.
Report on wellbeing, not just utilisation
When you talk to boards, payers or partners, show: “Here’s how our programs changed wellbeing scores, not just appointment counts.”
Trend 3 – Mental Health Crisis (NOW-NEW: 0-5 years)
What’s specific here?
The world is seeing a sharp, measurable rise in mental health problems. In the first year of COVID-19 alone, the global prevalence of anxiety and depression grew by about 25%, according to WHO. Recent national surveys show similar patterns – for example, in England, about 1 in 4 young people (16–24) now lives with a common mental health condition. (The Guardian, 2025)
At the same time, supply is not catching up: in many countries, over half of people who need help don’t get effective treatment. (BioMed Central, 2023)
Signals you’ll see in your organisation
Waiting lists that don’t go down
Long queues for psychiatrists, psychologists, child and adolescent services.
Primary care quietly absorbing a lot of mental health work.
More “mixed” cases
Mental health problems show up together with chronic disease, pain, substance use and social problems.
Harder to fit patients into neat diagnostic boxes.
Staff exhaustion
Clinicians feel they are “never enough” for the amount of need they see.
What to consider in the next 12–36 months
Redesign triage and care levels for mental health
Use stepped care: self-help → group / digital therapy → short-term therapy → specialist care.
Let digital tools and group formats handle mild and moderate cases so specialists can focus on severe ones.
Scale access with blended and digital care
Combine online CBT, group programs, chat support and brief visits instead of only long 1:1 therapy blocks.
Invest in platforms that can host these blended journeys in a structured way.
Treat mental health as part of every chronic care pathway
Systematically screen for depression and anxiety in diabetes, cardiac, oncology, pain and long COVID clinics.
Make psychological support part of the standard offer, not a rare add-on.
We built a patient management platform and an AI-powered data source for tailored care & deeper understanding of US minority communities.
Delivering a novel ethnic-aware patient care platform with AI & data science
Trend 4 – Burnout Society (NOW-NEW: 0-5 years)
What’s specific here?
Burnout is no longer just a niche topic in hospitals. It’s becoming a mainstream work-related condition across sectors. A recent review suggests that around one-third to almost half of healthcare and public health workers show signs of burnout. (BioMed Central, 2024)
Outside healthcare, large workforce studies find that the majority of workers report burnout symptoms, especially younger generations. (The Times)
Signals you’ll see in your organisation
Staff turnover and sick leave going up
More resignations, especially among nurses, junior doctors and frontline staff.
More sick days for stress, exhaustion and “unspecified” mental health reasons.
Lower quality and more errors
Burnout is linked to higher medical error rates, lower empathy and worse patient experience.
Teams struggle to maintain standards when constantly short-staffed.
Management time consumed by “firefighting people issues”
Leaders spend more time on rota crises, conflicts, last-minute replacements and exit interviews.
What to consider in the next 12–24 months
Measure burnout and workload honestly
Use short, anonymous surveys (e.g. 2–3 questions from validated scales).
Track burnout by department and role to see where the pressure is worst.
Fix obvious structural pain points before adding “wellness”
Review shift patterns, staffing levels, admin burden and IT friction.
Sometimes removing two pointless forms and one extra login does more for burnout than ten mindfulness workshops.
Design digital tools that reduce, not add, cognitive load
When you build or buy software, check:
how many clicks a common task takes,
whether it reduces double data entry,
whether it fits into actual workflow instead of fighting it.
Train and support line managers
Managers are often the first to see burnout signs.
Give them basic training and simple playbooks for conversations, adjustments and referral to support.
Trend 5 – Dehumanization of Relationships (NOW-NEW: 0-5 years)
What’s specific here?
We see more polarisation, online aggression, echo chambers and loneliness. People are connected technically, but social trust and the quality of conversation are often low. Family structures change, local communities weaken, and more people live alone. This shows up in rising loneliness figures in many countries – and loneliness is linked with higher risks of depression, heart disease and even early death.
Signals you’ll see in your organisation
Patients who don’t have anyone “to call”
More people without carers, partners or close friends who could help with medication, appointments or decisions.
Discharge planning gets harder because there is no family network to rely on.
More conflict and mistrust around care
Patients come in with strong, polarised views shaped by social media or niche communities.
Mistrust of institutions, vaccines, “the system” – and more confrontation with clinicians.
Clinicians feeling emotionally drained and “de-personified”
Being treated as “service providers” or “the enemy” rather than trusted professionals.
What to consider in the next 12–24 months
Include social connection in your assessments
Ask simple questions:
“Is there someone who can help you if you get sick?”
“How often do you feel lonely?”
Use this to flag high-risk patients who might need more follow-up and support.
Design services that also rebuild connection
Group visits, peer support groups, community-based programs and volunteers can become part of the model.
Digital platforms can host safe, moderated peer communities, not only one-to-one care.
Support clinicians in dealing with hostility and mistrust
Training in communication, de-escalation and handling conspiracy narratives.
Clear policies on abuse, plus psychological support after difficult encounters.
We built a secure, scalable API for a 10k-product healthcare database. Added automation and cloud-ready architecture.
We provided 19 functional API endpoints with a 2-developer team in just 3 weeks
Trend 6 – Society of the Addicted (NOW-NEW: 0-5 years)
What’s specific here?
Addictions are not limited to “classic” substances anymore. We have:
Substance use disorders (alcohol, opioids, stimulants, etc.),
Behavioural addictions (gambling, gaming, shopping, pornography),
Technology-related addictions (social media, mobile phones).
According to the latest global data, alcohol and drug use disorders, self-harm and interpersonal violence together create a huge and growing burden of disease, with high disability and death rates, and trends projected to stay high up to 2040. The UN World Drug Report warns that around 316 million people used drugs in 2023, up sharply over the last decade, with cocaine and synthetic drugs expanding fast. (WELT, 2023)
Signals you’ll see in your organisation
More patients with dual or triple diagnoses
Addiction plus depression, anxiety, trauma or chronic pain.
High use of emergency care, low adherence to treatment.
Hidden addictions in general patient populations
Alcohol overuse not mentioned unless you ask directly.
Gaming, gambling or shopping addictions showing up as sleep problems, debt, relationship breakdown.
High impact on admissions and costs
Frequent attenders with complications of alcohol, drugs or risky behaviour.
Hard-to-stabilise patients who cycle through the system.
What to consider in the next 12–36 months
Make basic addiction screening part of routine care
Short validated tools (AUDIT-C, brief drug use questions) in primary care, mental health and emergency settings.
Ask about behavioural addictions in a normal, non-judgmental way.
Integrate addiction treatment with mental and physical healthcare
Co-locate or tightly connect addiction services with mental health and chronic disease clinics.
Use case managers or care coordinators for high-risk patients.
Use digital tools to support recovery – with safeguards
Apps for craving tracking, contact with peer support, reminders, relapse prevention content.
Clear rules on data privacy and clinical oversight.
Partner beyond the clinic
Work with schools, employers, justice systems and community organisations to identify and support people earlier.
Cluster: Chronic disease & aging
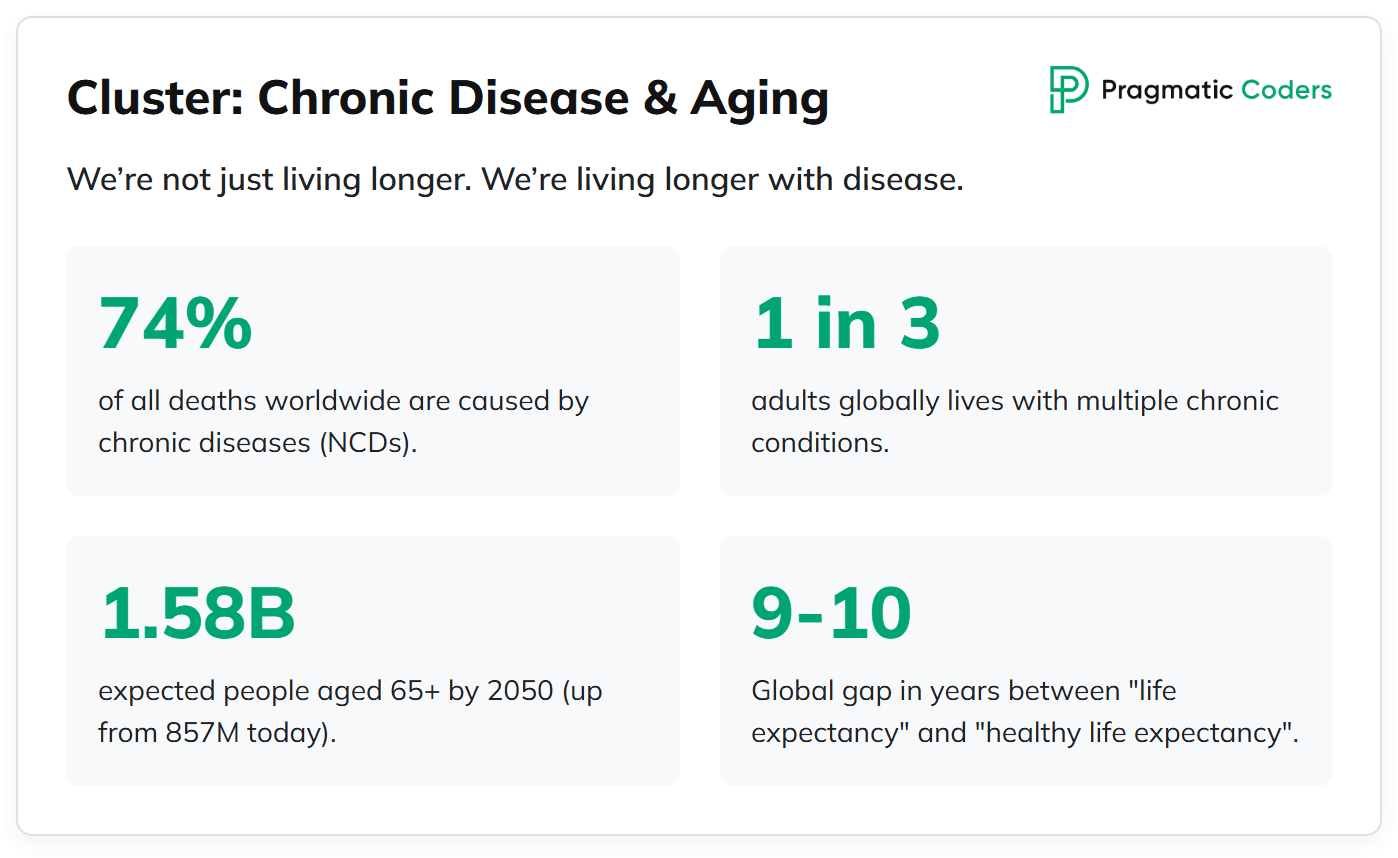
We’re not just living longer. We’re living longer with disease.
A few key facts to set the stage:
Chronic diseases (NCDs) – things like heart disease, cancer, diabetes, chronic lung disease – now cause about 74% of all deaths worldwide. In 2021 that was over 43 million people. (WHO. 2025)
A big share of these deaths are “premature” (before age 70), especially in low- and middle-income countries. (WHO)
Globally, about 1 in 3 adults lives with multiple chronic conditions at the same time (for example diabetes + hypertension + depression). (ScienceDirect. 2018)
In the US, recent data show that around 51% of adults have at least one chronic condition, and over half of midlife adults already have multiple – so this is no longer just an “old people” issue.
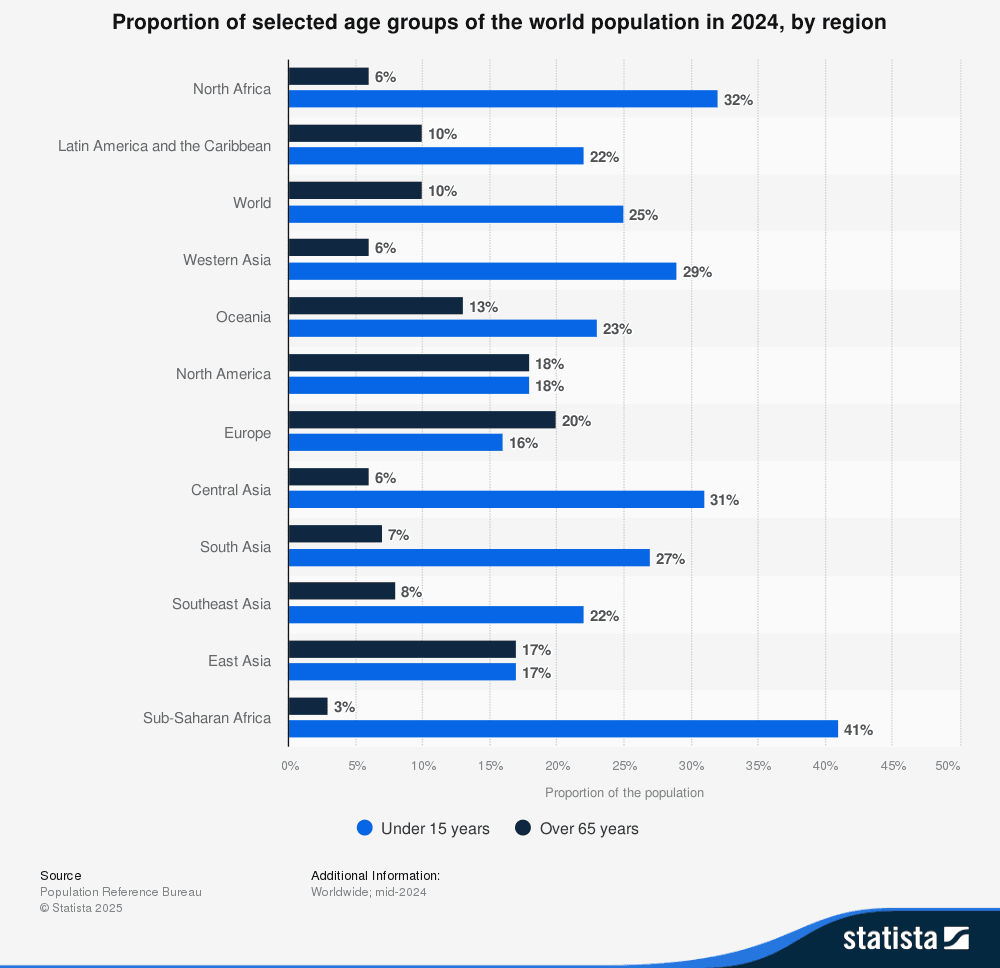
On the aging side:
Today there are roughly 857 million people aged 65+ in the world. By around 2050, that number is expected to jump to about 1.58. (Statista, 2025)
People live longer, but not proportionally healthier. Globally, the gap between life expectancy and “healthy life expectancy” is around 9–10 years – years lived with significant illness or disability. In the US it’s over 12 years. (JAMA Network, 2025)
Put simply: we’re heading towards a world where chronic disease is normal, most older adults live with several conditions at once, and many people spend a decade or more of life in poor health.
For healthcare leaders, this cluster (Society of the Chronically Ill, Aging Society, Wellaging, Elimination of Old Age, Epidemic of Brain Diseases) means:
Volume + complexity
More patients, living longer, with multiple linked conditions instead of one clear diagnosis.
Care plans, meds and risks all become more complex to manage.
Pressure on long-term care and financing
Systems built for short, acute episodes struggle with long, fluctuating, multi-year journeys.
Costs shift towards long-term management, not one-off hospital stays.
Huge opportunity in prevention, coordination and tech
If you can prevent just a fraction of complications, or delay them by a few years, the impact is massive.
Good data, coordination and digital tools become survival skills, not “nice extras”.
Trend 7 – Society of the Chronically Ill (NOW-NEW: 0-5 years)
What’s specific here?
“Society of the chronically ill” means that chronic disease becomes the default state, not the exception. Many people don’t have “one diagnosis”, they have 3–5: for example obesity, type 2 diabetes, hypertension, anxiety and osteoarthritis at the same time. As mentioned earlier, research suggests that around one in three adults globally has multiple chronic conditions, and this share rises sharply with age.
This changes everything: how people work, how they age, and how they use healthcare.
Signals you’ll see in your organisation
Most of your patients are “multi-condition” by default
Clinic lists where diabetes + hypertension + depression is normal, not rare.
Harder to tell which specialist “owns” the patient.
Frequent, unplanned use of care
Repeated visits and admissions for complications, flare-ups and side effects.
Emergency departments quietly turning into chronic care hubs for people who fall through the cracks.
Medication overload and confusion
Patients on 5, 10 or more medicines, with unclear priorities.
Non-adherence, dangerous combinations, and “I don’t know why I’m taking half of these”.
Quality of life as the real outcome
Even when you “control” numbers (blood pressure, HbA1c), many people still feel tired, limited, in pain or low in mood.
Success is less about “cure” and more about function, independence and meaning.
What to consider in the next 12–36 months
Shift from single-disease programs to multi-condition care
Instead of completely separate pathways for diabetes, heart failure, COPD, etc., design integrated clinics or teams for people with 2+ conditions.
Make one person or team clearly responsible for overall coordination, not just each silo.
Use risk stratification and registries, not just waiting rooms
Build (or commission) simple tools that:
list all patients with multiple chronic conditions,
flag those with recent admissions, poor control or social risk,
support proactive outreach rather than waiting for crises.
Prioritise medication review as a core service
Regular, structured polypharmacy reviews for older and high-risk patients.
Simple goals:
reduce unnecessary drugs,
simplify regimens,
align meds with what matters most to the patient (pain, function, cognition, etc.).
Make self-management and digital support the “first line”, not an afterthought
Apps, portals, telemonitoring and remote coaching can:
help track symptoms and vitals,
nudge activity, diet and meds,
catch early warning signs before a hospital visit.
For many organisations, this will mean building or customising a platform rather than relying only on generic tools.
Bring mental health into every chronic care pathway
Systematically screen for depression, anxiety and cognitive issues in people with multiple conditions.
Offer at least basic psychological support or digital CBT options inside chronic programs.
| Custom Telemedicine Software Development We create cutting-edge telehealth platforms to connect patients and providers seamlessly. Discoverr our custom telemedicine solutions. |
Trend 8 – Aging Society (NOW-NEW: 0-5 years)
What’s specific here?
Populations are getting older, fast. The share of people 65+ is expected to move from about 9–10% in 2022 to over 16% by 2050 (National Library of Medicine, 2022). So almost every health system is turning into a geriatric system, whether it’s ready or not.
Signals you’ll see in your organisation
Your “average” patient is older and more complex
More people 70, 80, 90+ with multiple conditions, frailty and social needs.
More cognitive issues, falls, polypharmacy and functional decline.
Demand shifts from acute rescue to long-term support
Less “single episode” care, more recurrent visits, home care and rehab.
More pressure on long-term care, nursing homes and family carers.
Workforce and financing strain
Fewer working-age people per older person.
Growing gap between what older adults need and what systems can fund and staff.
What to consider in the next 12–36 months
Make geriatric thinking “default”, not a niche specialty
Train non-geriatric clinicians in basics: frailty, delirium, polypharmacy, falls, cognitive assessment.
Build simple tools in your EHR platform to flag frailty and fall risk as early as possible.
Redesign care around function, not just disease codes
Ask routinely about mobility, daily activities, continence, cognition, mood, social support.
Use those answers to guide priorities and resource allocation.
Invest in models that keep older adults at home longer
Hospital-at-home, remote monitoring, home rehabilitation, teleconsults.
Coordinate with social care and community services instead of working in a silo.
Use technology to support carers as well as patients
Portals and apps for family caregivers: medication lists, alerts, education, shared care plans.
Trend 9 – Wellaging (NEW-NEXT: 1-15 years)
What’s specific here?
“Wellaging” flips the focus from “how long can we keep people alive” to “how long can people stay healthy and independent”. Globally, life expectancy and healthy life expectancy have both risen since 2000, but the gap between them is around 9–10 years – years lived with significant illness or disability. Recent work shows that in the US this gap is even larger, over 12 years and among the widest in the world (JAMA Network, 2025).
So the key question becomes: how do we compress those “bad years” at the end of life?
Signals you’ll see in your organisation
Patients care more about independence than lab values
Older adults ask: “Will I still be able to walk, drive, live at home?” more than “What’s my exact number?”.
Quality of life, mobility and cognition become central outcomes.
More interest in prevention and lifestyle at older ages
People in their 50s, 60s, 70s asking what they can do now to avoid dementia, disability and nursing homes.
Payers and policy makers start talking about “healthspan”
They want to see fewer years of high-cost, high-dependency care, not just lower mortality.
What to consider in the next 12–36 months
Define “healthy aging” metrics for your population
Track simple outcomes: falls, hospitalisations, days at home, mobility levels, basic ADLs (activities of daily living).
Use these measures alongside classic disease indicators.
Build programs that delay disability, not just manage disease
Multicomponent interventions: strength and balance training, nutrition, medication review, vision/hearing checks, cognitive stimulation.
Integrate them into primary care and chronic disease clinics.
Offer midlife (40–65) “future health checks”
Assess cardiovascular risk, metabolic health, sleep, mental health, activity, cognitive risk factors.
Provide personalised plans and digital follow-up – this is where custom platforms and AI coaching can shine.
In just six weeks, we built a platform that ensured the safety of WithHealth's clients' workforce during the COVID-19 pandemic.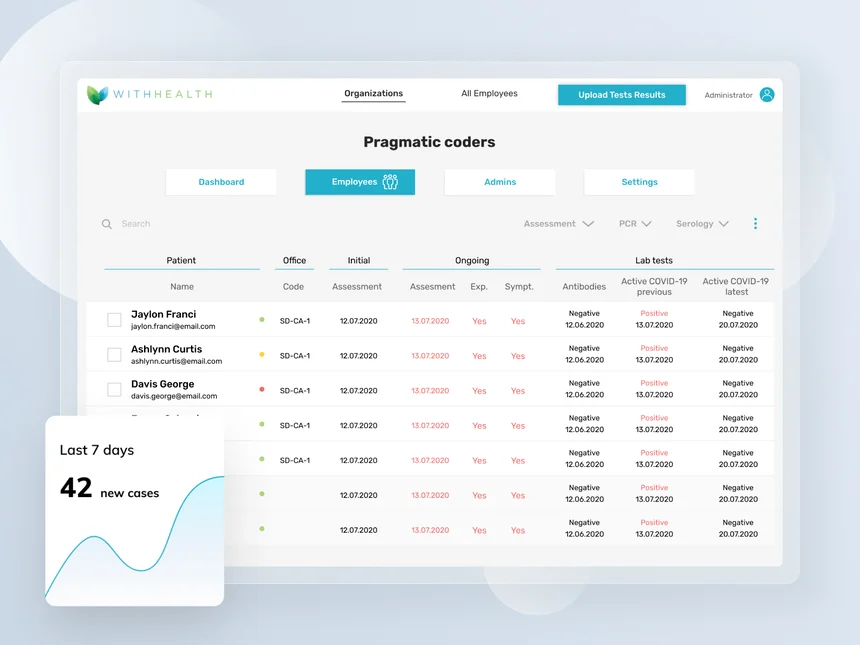
WithHealth: Launching a patient MedTech portal in six weeks
Trend 10 – Elimination of Old Age (NEW-NEXT: 1-15 years)
What’s specific here?
This trend is about efforts to delay, slow or even reverse biological aging. It includes areas like:
geroscience (targeting aging pathways),
drugs that act on aging mechanisms (e.g. senolytics, metformin trials, rapamycin analogues),
longevity biotech and “age-reversal” startups.
Researchers and organisations are exploring the idea that aging itself could be treated like a risk factor or even a disease, not just a background condition. Some projections suggest that tackling aging biology could add many healthy years at the population level, but most of this is still experimental and unevenly regulated.
Signals you’ll see in your organisation
Patients asking about “longevity drugs” and age tests
Interest in biological age tests, supplements, off-label use of drugs, gene therapies in the media.
Wealthy or tech-savvy patients may arrive with “longevity protocols” they already follow.
Growth of private longevity clinics and services
Advanced diagnostics, personalised prevention packages, often cash-paid and outside mainstream systems.
Ethical and equity questions
Who gets access if effective age-slowing interventions appear?
Risk of widening health gaps between those who can and can’t pay.
What to consider in the next 12–36 months
Prepare clear, evidence-based communication
Clinicians need simple messages about what is proven, what is promising and what is hype.
Build short internal summaries and patient-facing materials.
Focus on “boring” but powerful longevity basics
Activity, diet, sleep, blood pressure, glucose, smoking, alcohol – still the biggest levers for healthspan.
Align your prevention programs with this, even as you watch emerging geroscience.
Decide your stance on longevity services
Will your organisation:
ignore them,
partner with selected providers,
or build its own evidence-based offer?
Start by defining ethical, clinical and data standards you won’t compromise on.

Trend 11 – Epidemic of Brain Diseases (NEW-NEXT: 1-15 years)
What’s specific here?
Neurological disorders – especially dementia and Parkinson’s disease – are rising fast as populations age. WHO estimates that around 57 million people were living with dementia in 2021, with almost 10 million new cases every year; this number is expected to grow sharply as societies age (The Times of India, 2021).
Global studies show that the burden of Alzheimer’s disease and other dementias has increased over the last decades, and age-standardised rates for several neurological conditions are also rising (Journal of Global Health, 2023). Parkinson’s disease is now the second most common neurodegenerative disorder, and WHO estimates that neurodegenerative diseases like Alzheimer’s and Parkinson’s could become the second leading cause of death worldwide by around 2040, surpassing many cancers. (Bmj research, 2024).
Signals you’ll see in your organisation
More patients with cognitive and movement problems in every clinic
Dementia and mild cognitive impairment showing up in primary care, cardiology, diabetes, oncology – not just neurology.
Increasing numbers of older adults with Parkinson’s or parkinsonian symptoms.
Families under heavy pressure
Dementia and other brain diseases put huge emotional and financial strain on carers.
More need for respite care, guidance and coordination, not only medication.
Systems that are not built for long, complex neuro journeys
Fragmented pathways between neurology, psychiatry, geriatrics, primary care and social care.
Long waits for diagnosis and patchy access to rehab and support.
What to consider in the next 12–36 months
Normalise early detection of cognitive and neurological issues
Add short cognitive checks and basic neuro questions for older patients in primary care and chronic clinics.
Clear pathways: what happens after a positive screen, how fast, and where.
Build integrated brain health pathways
Combine neurology, psychiatry, geriatrics, rehab and social care in more joined-up services.
Use coordinators or case managers for people with dementia and advanced Parkinson’s.
Support carers as a core “target group”
Training, psychoeducation, helplines, support groups, digital tools for caregivers (reminders, shared calendars, resources).
Recognise that supporting carers can prevent crises and hospitalisations.
Track and prepare for new diagnostics and treatments
Blood tests and imaging biomarkers for Alzheimer’s, new disease-modifying drugs, neurotech tools.
Decide how and when your organisation will adopt them: criteria, capacity, funding, ethical guardrails.
Cluster: Human+ & advanced medicine
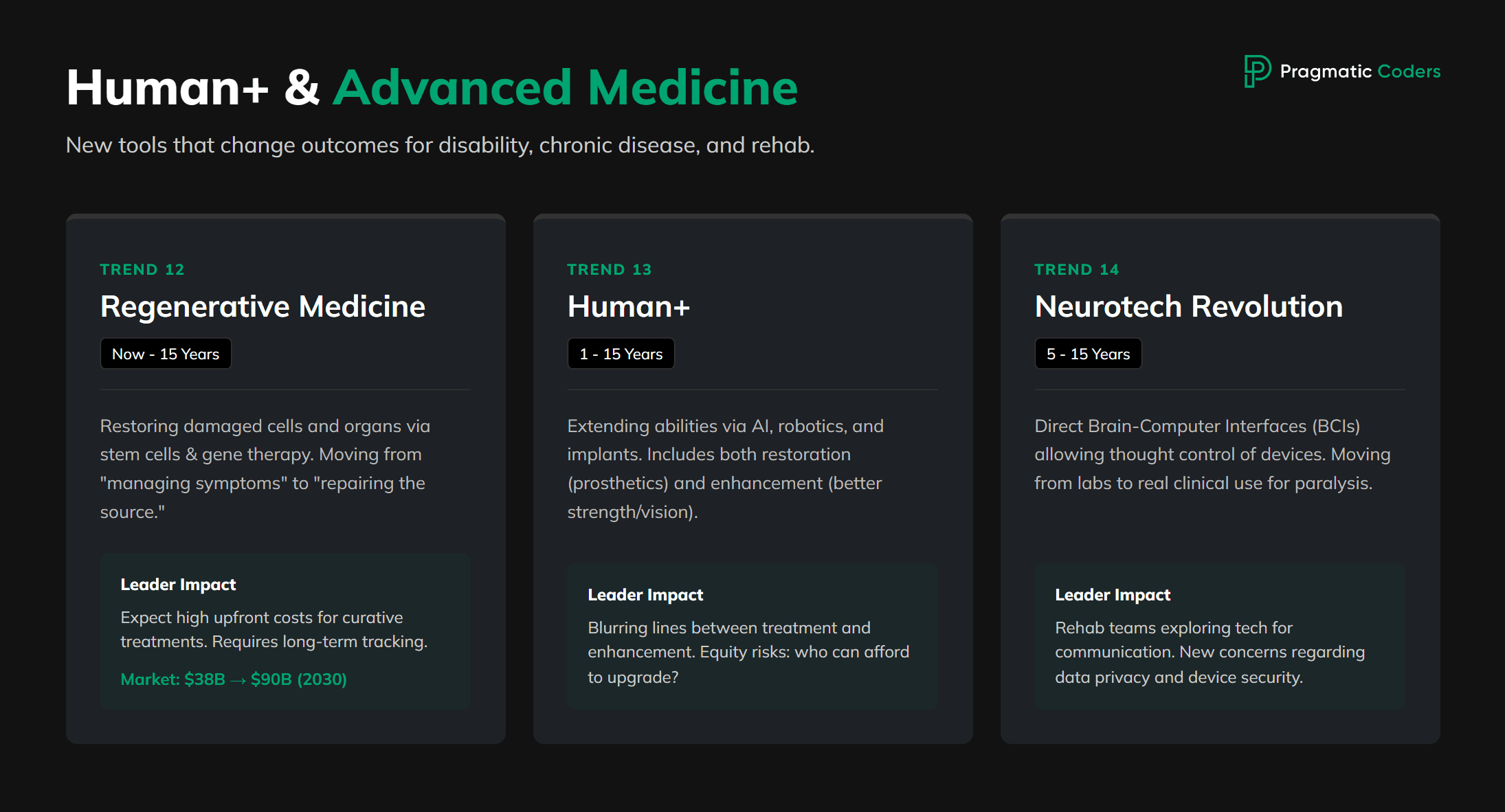
Here we’re talking about medicine that doesn’t just treat disease, but adds new abilities or restores lost ones in ways that feel almost sci-fi:
Regenerative medicine – repairing or replacing cells, tissues and organs.
Human+ – enhancing human abilities with AI, robotics, implants and biotech.
Neurotechnological revolution – brain–computer interfaces and neuroimplants.
A few anchors:
The regenerative medicine market is expected to grow from around USD 38 billion in 2025 to almost USD 90 billion by 2030, driven by stem cells, gene therapies and tissue engineering. (Mordor Intelligence, 2025)
The broader implantable devices market – pacemakers, neurostimulators, joint replacements and more – is already worth well over USD 100 billion and is projected to roughly double by the mid-2030s. (Global Market Insights, 2025)
Neurotech is moving fast: we now have BCIs in clinical trials that let people with paralysis control devices, communicate and even operate smart homes using only their thoughts. Several companies, including Neuralink, Synchron and Paradromics, have already tested implants in humans.
For healthcare leaders, this cluster is about:
New tools that can radically change outcomes – especially for disability, chronic disease and rehab.
New safety, ethics and equity questions – who gets access, who pays, what happens to data, how far do we go?
New expectations from patients – people will arrive asking about gene therapy, implants and enhancement, not just pills and surgery.
Trend 12 – Regenerative Medicine (NOW-NEW-NEXT: 0-15 years)
What’s specific here?
Regenerative medicine aims to restore or replace damaged cells, tissues and organs, instead of only managing symptoms. It uses tools like stem cells, gene therapies, tissue engineering, biomaterials and 3D bioprinting. The global market is growing fast – estimates suggest it could more than double between 2025 and 2030, reaching around USD 90 billion. (Mordor Intelligence, 2025)
Today, real-world use includes things like:
cell and gene therapies for blood cancers and some rare diseases,
skin and cartilage regeneration,
experimental work in heart, nerve and muscle repair.
Signals you’ll see in your organisation
More referrals and questions about advanced therapies
Patients and clinicians asking about cell and gene therapies, lab-grown tissues, experimental regeneration trials.
Complex, expensive one-time treatments
Very high upfront costs, but potential for long-term benefit or cure.
New contracting and reimbursement models (“pay for outcome over years”).
Data and follow-up requirements
Long-term registries to track safety and durability of effects.
Need for tight coordination between specialist centres and local providers.
Trend 13 – Human+ (NEW-NEXT: 1-15 years)
What’s specific here?
“Human+” is about extending human abilities with technology: AI, robotics, implants, exoskeletons, gene and digital engineering. Some of this is restorative (e.g. cochlear implants, robotic prostheses), some of it is enhancement (stronger, faster, smarter than before). Global implant markets and neurotech advances show that this is no longer science fiction – it’s already shaping rehab, surgery, chronic care and disability support.
Examples today:
Pacemakers and implantable defibrillators keeping hearts in rhythm for millions.
Cochlear implants giving hearing to people with severe deafness.
Robotic limbs and exoskeletons helping people walk and lift again.
AI decision support helping clinicians read scans and choose treatments.
Signals you’ll see in your organisation
More patients living with complex tech “inside or around” their body
Implanted devices, wearables, home robots, advanced prostheses.
Need for device management, software updates, security and data handling.
Blurring line between treatment and enhancement
People wanting to go “beyond normal” – better vision, strength, cognition or endurance.
Demands for access that go beyond classic medical indications.
Equity and ethics questions
High-cost tech risks creating a two-speed system: those who can upgrade and those who can’t.
Trend 14 – Neurotechnological Revolution (NEXT: 5-15 years)

Neuralink chip
What’s specific here?
Neurotechnology covers brain–computer interfaces (BCIs), neuroimplants, deep brain stimulation, advanced brain imaging and stimulation tools. It’s moving quickly from labs into clinical practice:
Clinical BCIs already allow people with paralysis to control cursors, type messages and operate smart home devices using only their thoughts.
Companies like Neuralink and others have implanted devices in humans to help restore communication and movement, and are exploring vision restoration and other functions.
These tools can restore function after stroke, spinal cord injury or neurodegenerative disease, but they also raise deep questions about identity, privacy and autonomy.
Signals you’ll see in your organisation
More patients with implanted neuro devices
Deep brain stimulators for Parkinson’s, spinal cord stimulators for pain, experimental BCIs for paralysis.
Complex interactions between hardware, software, meds and rehab.
Growing interest from rehab teams and patients
Physiatrists, neurologists and therapists asking: “Can neurotech help this patient walk, speak or communicate again?”
Families searching online for BCI trials and neuroimplants.
New kinds of risk
Device failure, hacking concerns, unwanted changes in mood or personality, unrealistic expectations.
Conclusions
The big picture is hard to ignore: healthcare is moving toward an AI-centered future. Because when elderly patient volumes rise, conditions get more complex, and care shifts online, only AI-powered systems can keep up with the scale and speed modern medicine demands.
If you want to build software that’s ready for that future — from patient platforms to AI-driven care coordination — check out our AI healthcare software development services. We help healthcare organizations turn these trends into real solutions.